Your Colorectal Health, Our Priority
With our comprehensive suite of screening services and treatment options, our experienced colorectal specialist and medical team promise you peace of mind whilst ensuring a strong and healthy colon.


What Is TheColon And Rectum?
The colon and rectum together form the large intestines. The last 15cm of the large intestines is known as the rectum, while the rest of it is called the colon. This is the last part of the digestive system. The small intestine is responsible for most of the digestion of food and absorption of nutrients. Whatever that is not absorbed, passes into the colon, where most of the water is absorbed by the body.
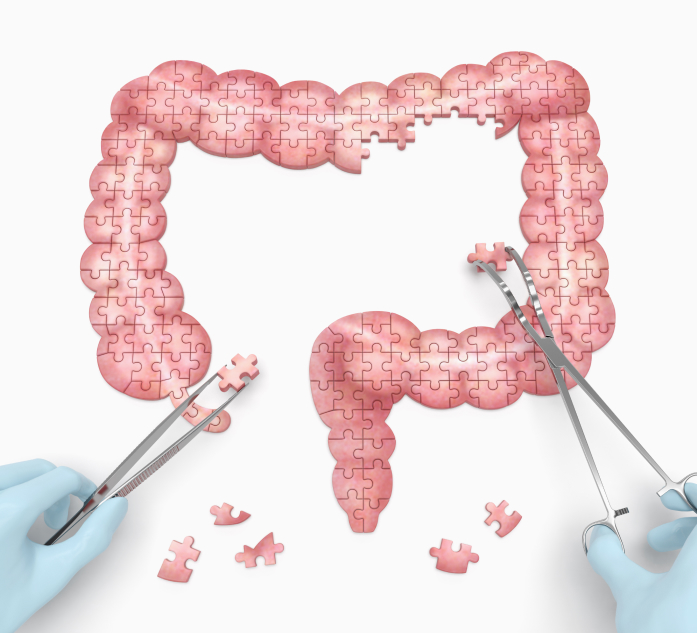
What Conditions Require Colon And Rectum Surgery?
Majority of the colon and rectum surgery done in Singapore are for colon and rectal cancer. Less frequently, they are performed for conditions such as diverticular disease, ulcerative colitis, Crohn’s disease, chronic constipation or rectal prolapse.
Colon surgery is almost always performed through the abdomen. In suitable cases of rectal surgery, the surgery is performed through the anus.
Our colorectal surgeon has two decades of experience in the field and is committed to ensuring that all surgical treatments are well-tailored to each individual.
With minimally invasive surgery, you can rest assured that your recovery will be faster and more comfortable, with less scarring and reduced risk of complications.
Step By Step Guide To Colon And Rectum Cancer Surgery
1. Before Surgery
As the surgery is most commonly performed under general anaesthesia, your colorectal surgeon will likely arrange for some blood test, electrocardiogram (ECG) and chest x-rays before surgery. This is to ensure that you are fit for surgery. Your anaesthetist may also see you before the surgery if required. For cancer surgery, a CT scan may also be done to give more detailed information about the location and its extent of spread before surgery.
You will be required to fast for 6 hours before the surgery. Medication will also be given to clear the bowel of any residual faeces. An intravenous drip may also be given to ensure adequate hydration during the period of fasting.
2. During Surgery
After anaesthesia, body hair over the site of surgery will be shaved off. A tube will also be inserted into the bladder to drain out the urine during surgery. Sometimes, a tube will also be inserted through the nose into the stomach to drain out the excess air and fluid in the stomach.
3. Immediately After Surgery
When you wake up from anaesthesia, the tubes that are inserted would be in place. Pain killers should have already been administered so there will not be much pain.
4. After Surgery
It is normal that the stomach and intestines stop functioning for up to 48 hours after colon and rectum surgery. During this period, oral intake will be restricted. Pain killers will be administered via intravenous infusion.
The tube inserted into the bladder will usually be removed after two or three days when you are ready to get up and go and pass urine on your own. The stomach tube, if inserted, is usually removed on the first or second day.
As the intestine function slowly recovers, your surgeon will progress your oral intake from water to soft diet and eventually to solid foods. Once you are able to eat and pass motion, you are ready to go home.
5. Upon Discharge
Please resume normal daily activities upon going home. The wound requires minimal care and it is alright even if it gets a bit wet during a bath. You are advised to refrain from strenuous activities for one to two months after surgery to allow the muscle wound to heal properly.
For more information about colon and rectum surgery, please visit our Singapore Colonoscopy Clinic website.
Our Colorectal SurgeonColorectal Specialist

Dr Ho Kok Sun
Consultant Colorectal & General Surgeon
MBBS (Singapore), M Med (General Surgery) (Singapore)
FRCS (General Surgery) (Edinburgh), FAM (Singapore)
Dr Ho Kok Sun has been treating all colon and rectal conditions for over a decade and was the past President of the ASEAN Society of Colorectal Surgeons and the Society of Colorectal Surgeons (Singapore), as well as a founding member of the Eurasian Colorectal Technologies Association. Dr Ho was actively involved in the training of medical students and residents, and has published widely in reputable journals and book chapters. He believes that treatment should always be personalised to the patient’s needs.

